Turning off the baby shower: the future of male contraceptives
Expert reviewers
Laureate Professor John Aitken
Pro Vice-Chancellor, Office of the PVC Health and Medicine (Biological Sciences)
The University of Newcastle
Essentials
- Condoms or a vasectomy are the only contraceptive options currently available for men.
- There are commercial impediments to the development of new male contraceptives.
- Future male contraceptives would need to be effective, safe, reversible and acceptable.
- There is ongoing research into hormonal and non-hormonal contraceptives for men, with hormonal options currently the most promising.
- Future contraceptives for men could work by stopping the production of sperm, blocking its pathway and/or affecting its ability to fertilise the egg.
It’s been 50 years since the oral contraceptive pill became available for women. Today, women have a lot of options when it comes to contraception—from intrauterine devices (IUDs) and vaginal rings to hormonal implants and injections. By contrast, there have been no new contraceptives for men on the market during the whole of the twentieth century.
Apart from traditional (and hardly fail-safe) methods like withdrawal GLOSSARY withdrawalejaculating outside the vagina or the rhythm method GLOSSARY rhythm methodlimiting sexual intercourse to the infertile phases of the woman’s menstrual cycle , men have two options: use a condom or have a vasectomy. Both have their problems. Condoms are very effective—when used perfectly. But throw a bit of human fallibility into the mix and they can have a pretty high failure rate. A vasectomy, on the other hand, is an extremely effective form of contraception, but is designed to be permanent.
Among current male contraceptive methods, the reversible methods are not reliable and the reliable method is not intended reversible.Professor David Handelsman (topic reviewer)
When it comes to male contraception, are condoms or vasectomies as good as it gets? For a long time we’ve been hearing that male contraception is just around the corner. So where are these alternatives?

Why aren’t there more options for men?
When we consider why there are so many more options available for women than men, it’s tempting to assume the barriers are technical. After all, men produce a lot more sperm than the one egg a month released by women. Are there just too many sperm for a male contraceptive counter? Is coming up with a new, effective male contraceptive simply too difficult? Not at all. In fact, as we’ll see, there has been extensive research in the area of male contraception, with many promising developments, especially in hormonal methods.
The main barrier to the availability of new methods of male contraception lies elsewhere: in the reluctance of major pharmaceutical companies to invest in developing what they perceive as low profit, potentially high-risk drugs for healthy people, preferring to develop drugs in more lucrative and less risky areas of chronic disease. Part of the problem may be the perception that not many men would use (and buy) new male contraceptives. Yet, interestingly, surveys across a number of countries indicate that over 50 per cent of men may be willing to take a male Pill if available, and that female partners would trust them to take it.
In the absence of commercial interest, some non-profit groups and public-sector organisations, such as the World Health Organization, CONRAD (Contraception Research and Development), the Population Council (which developed the Mirena IUD for women) and the Parsemus Foundation are carrying out research and development in this area.
To be feasible, any new male contraceptive would need to be:
- effective—in preventing pregnancy
- safe—with no major or unacceptable side effects
- reversible—so that fertility could be restored when desired
- acceptable or user-friendly—so that men would be willing to use it and so that their partners could rely on it.
How does male contraception work?
Essentially, male contraceptives being researched target sperm. They do this by:
- interfering with their production or development
- physically blocking their passage to the egg
- affecting their ability to fertilise the egg (for instance, by affecting their swimming ability or ability to bind to the egg).
Incorporate one or more of these steps on the sperm’s journey, and you could potentially have a workable contraceptive for men.
Hormonal contraception
Of the various developments in male contraceptives, hormonal methods are the most promising. Scientists in the academic sector have carried out early stage clinical development and have shown hormonal contraceptives to be reliable, reversible, safe and acceptable.
It’s worth noting that, while this kind of contraception for men is sometimes referred to as a male Pill (because, like the oral contraceptive pill for women, it works by introducing hormones into the body), hormonal options for men would take the form of an injection or implant. This is because, if taken orally, much of the testosterone is quickly broken down by the liver and can also cause liver damage.
How do hormonal contraceptives for men work?
Traditional, exiting methods of male contraception (condoms and vasectomy) are mechanical in nature—that is, they work by introducing a physical barrier. Hormonal contraceptives for men, on the other hand, work in a similar way to hormonal contraceptives currently available for women. In women, hormonal contraceptives suppress signals from the pituitary GLOSSARY pituitarya pea-sized, hormone-producing gland in the brain gland in the brain to the ovaries, preventing the egg from maturing, so that women don’t ovulate and can’t get pregnant. In men, they interfere with the production of sperm by acting on the messages sent between the brain and the testes. Put simply, they signal to the hormone-producing parts of the brain that they should stop making the hormones that promote the production of testosterone and sperm. The goal is to reliably switch off the production of sperm. It’s usually around three months before sperm will be washed out completely, similar to a vasectomy.
Contraceptives for men which include the hormone testosterone, for example, introduce a dose of testosterone into the body, with the result that the amount of testosterone in the bloodstream is more than is usually found there. This tricks the pituitary gland into thinking that there is enough testosterone in the body. In response, it suppresses the production of hormones which would usually trigger the making of testosterone and sperm.
There are three main kinds of hormonal contraceptives for men, each containing different hormones or hormone combinations. These are:
- androgen only
- combined progestin and androgen
- GnHR antagonist and androgen.
Let’s take a closer look.
Androgen only
Androgens are sex hormones which give men their male characteristics (such as facial hair) and have a key role in male fertility. The main and best known one is testosterone. As we’ve just seen, contraceptives containing testosterone work by signalling to the pituitary that it should suppress the production of hormones that trigger the making of sperm.
The World Health Organization carried out two large-scale multinational studies of androgen contraceptives (one in 1990 and one in 1996), with Australian researchers playing a key role. Over 670 men from 16 centres in 10 countries received weekly injections of a contraceptive containing a form of testosterone (called testosterone enanthate). The study found that the contraceptives dramatically lowered sperm production and that supressing the production of sperm to very low levels resulted in a very effective form of contraception (that is, it’s not necessary for sperm count to be reduced to zero for pregnancy to be prevented). However, these very low levels of sperm were not achieved consistently across all men. Though it’s not really known why, Caucasian men, for example, are less likely than their Chinese counterparts to achieve the necessary low levels of sperm using an androgen-only contraceptive. They may need to use a contraceptive which, in addition to testosterone, includes another hormone called progestin.
Researchers are looking into various kinds of new testosterone products to determine which might be the most reliable, safe and acceptable. They’re also investigating different possibilities for getting them into the body. Weekly injections of testosterone, for example, are not exactly user friendly! However, newer androgen products that only need to be injected every 2 to 3 months appear to work well when combined with progestin.
Progestin plus androgen
A second hormonal option is combining the use of androgen with progestin. Progestins are synthetic versions of a hormone called progesterone. While progesterone has important functions in pregnancy in women, it has no known role in men.
Progestins are widely used in female contraceptives to help stop ovulation. Contraceptives for men which contain progestin work in a similar way—by signalling to the pituitary not to make the hormones which trigger the production of testosterone and sperm. If men use only progestin, however, the result is androgen deficiency, including impotence. For this reason, men using progestins need to take them in combination with an androgen such as testosterone so that they retain their sexual function and male characteristics.
Work by Australian scientists first proved that this combined approach was a feasible way forward. As with androgen-only contraceptives, however, research is ongoing into the best way to deliver progestin plus androgen contraceptives so that they will be effective and acceptable.
GnRH antagonist plus androgen
A third area of investigation is the use of injectable drugs that target something called gonadotropin-releasing hormone—GnRH for short. As with progestin, these are used with androgen (usually testosterone) so that men retain their male characteristics.
GnRH is made in the hypothalamus, a hormone-producing part of the brain. Usually, GnRH stimulates the release of a hormone from the pituitary gland. This hormone then binds to receptors GLOSSARY receptorscell surface receptors are proteins on the surface of a cell which allow communication with the outside world. Molecules outside the cell react with the receptor to cause changes in the cell. in the testicles, triggering sperm production. GnRH antagonists interrupt this process by binding to the receptors that natural GnRH would normally bind to, blocking them. As a result, when used together with testosterone, sperm output is very effectively suppressed.
Long-acting injections of GnRH antagonists plus testosterone are a promising possibility for male contraception. However, it’s unlikely to be as cost effective as progestin.
Non-hormonal contraception
As we’ve seen, hormonal contraceptives work by interfering with the production of sperm. Non-hormonal contraceptives for men, on the other hand, can work in a number of ways. Different kinds of non-hormonal contraceptives target sperm at different stages on its journey to the egg—from interfering with its production and development to affecting its ability to fertilise the egg.
Interfering with sperm production and development
Bye-bye Vitamin A
It’s been known for some time that dietary Vitamin A (retinol) is needed for normal sperm production. Past research has shown that Vitamin A deficiency in male rats leads to sterility. So one way researchers think they may be able to stop sperm being made is by targeting the production of retinoic acid, which is made in the body from Vitamin A, in the testis.
In particular, scientists have been looking at a receptor called retinoic acid receptor α. As the name suggests, it’s a receptor for retinoic acid. Researchers at Colombia University carried out experiments in which they gave mice drugs which targeted this receptor. Not only did this cause infertility but, importantly, the mice stayed healthy and the effect was reversible. The long-term effects on people, however, aren’t yet known. And, because Vitamin A is needed throughout the body for cells to divide properly, it’s important that contraceptives which target it do so very precisely so that there are no serious side effects.
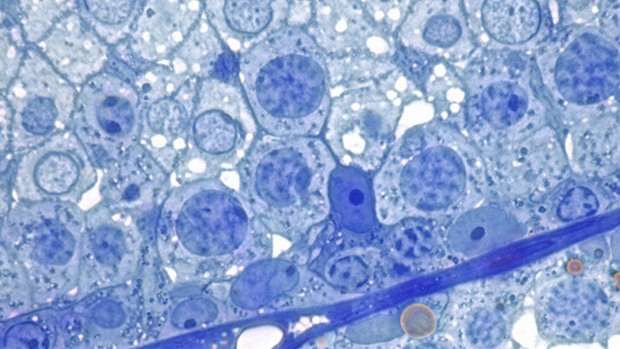
Targeting ‘nurse’ cells
Another approach is to use drugs which home in on special cells, known as Sertoli cells, in the testes. A Sertoli cell is a tall, column-shaped cell found in the wall of the seminiferous tubule—the place where male sex cells are created. Sertoli cells are what’s known as ‘nurse’ cells—they help in the production of sperm by supplying the nutrients, hormones and chemicals needed by the developing sperm. Men who don’t have Sertoli cells are infertile, so targeting them could be promising for male contraception. An advantage of drugs that target Sertoli cells is that they may be able to be taken orally.
One example, being developed by the Population Council, is a chemical called Adjudin. It stops young sperm cells from sticking to Sertoli cells—and, without Sertoli cells, the sperm can’t develop. However, when taken by mouth, a large dose of the chemical is needed for it to work effectively, leading to side effects in the muscles and liver. Scientists are now looking into better formulations—by making a more potent version, they hope a smaller, and safer, dose will do the job. As with drugs that target retinoic acid, research is still in its early stages.
The role of the epididymis
Other research is looking at proteins which are produced in the epididymis, the tube that joins the testicle to the vas deferens. It’s here that sperm get their ability to swim, and to recognise and bind to the egg. Scientists are working on identifying and targeting proteins made in this small, but significant, area which sperm need to develop. Stop sperm from developing properly, they reason, and you may well have an effective form of male contraception.
Some Australian scientists, for instance, have been examining a set of proteins activated in the epididymis that help sperm bind to the egg. While some men may have sperm which swim like champions, they may still be infertile if they lack a special ‘chaperone’ protein (called HSP2A), which helps sperm recognise and stick to the egg. Better understanding the role of this protein could not only help us better understand male fertility but, by targeting it, develop new contraceptives for men.
Another approach involves mimicking proteins which slow sperm down. Eppin is a protein covering the sperm’s surface. Normally, another protein called semenogelin, found in seminal fluid, binds to Eppin and stops the sperm from swimming. The sperm only get going again when an enzyme called PSA removes the semenogelin protein, allowing it to swim towards the egg. Researchers have been working on a drug which mimics the effect of the semenogelin protein and, importantly, isn’t removed by the PSA enzyme.

Stopping sperm in its tracks
What about physically blocking sperm on its journey to the egg?
A kind of sperm ‘roadblock’ is one option being looked at for a number of potential new contraceptives for men. A physical barrier (such as a polymer gel) is injected into the vas deferens (the duct which carries sperm from the testis to the urethra) so the sperm is blocked from continuing on its journey to the ejaculatory ducts.

By blocking the vas, these methods work the same way as a vasectomy. However, whereas in a vasectomy the vas are cut and sealed—making it a pretty permanent solution and very difficult to reverse—these blocking devices may be removed (for example, by a second injection that flushes out the gel). That means that fertility could potentially be restored—however, this is yet to be conclusively proven.
RISUG (Reversible Inhibition of Sperm Under Guidance) is one such approach, developed in India. Another, based on the Indian model, has been developed by the non-profit Parsemus Foundation in the United States. A polymer hydrogel (which they’re calling Vasalgel) is injected into the vas deferens in a non-surgical procedure performed under local anaesthetic. Sperm are too big to make it through the gel barrier, so are blocked from reaching the seminal fluid. The sperm is then absorbed back into the body. Human trials are scheduled to begin in 2016—but, as it hasn’t yet been shown that the procedure is fully reversible in large animals, people will participate on the understanding that infertility would be permanent.
Affecting sperm’s ability to fertilise to the egg
Rather than stopping the production of sperm, or blocking its pathway, what if we could step in at the end of its journey and impede its ability to fertilise the egg?
Promising research along these lines is looking at ways to stop sperm going into a special state called ‘hyperactivation’—which it needs to reach and burrow into the egg. Usually, as the sperm reaches the egg, its swimming pattern changes: it starts lashing its tail about wildly, like a (slightly deranged) freestyler going for gold. This frantic movement is triggered by the release of progesterone by the egg. A rush of calcium goes into the sperm’s tail, enabled by the opening of a calcium channel (a kind of ‘gate’ which lets electrically charged ions enter the sperm) known as CatSper GLOSSARY CatSpershort for ‘cation channels of sperm’—channels whose functions include controlling the flow of electrical signals across the cell. . Scientists are looking into potential drugs which could block the action of CatSper—and potentially be a new form of male contraception.
Fertile ground for research
From hormone injections to polymer gels, there are a lot of possibilities for future male contraceptives. So—is a new male contraceptive just around the corner? We’ll just have to wait and see. In the meantime, research in this area may not only provide avenues for potential new contraceptives, but also may help us better understand male fertility—and infertility.