Immunisation—protecting our children from disease
Expert reviewers
Essentials
- Vaccination represents the most successful form of disease prevention.
- Vaccines can control, eliminate and eradicate diseases.
- There is huge economic, as well as health benefits to vaccination.
- Vaccines can protect not only individuals but whole communities.
- Vaccine technology continues to improve, resulting in safer and more effective vaccines against a broad range of infectious diseases.
Immunisation is one of the great scientific advances that has changed the world as we know it. It is an affordable and effective means of protecting not just individuals but whole communities from debilitating diseases.
Many childhood diseases can spread very quickly and have serious consequences. Vaccination is one of the key ways of reducing the incidence of infectious diseases. But what actually is immunisation? Is it safe? What is in a vaccine? How does it work and why is effective?
What is immunisation?
Immunisation is the process whereby an individual’s immune system GLOSSARY immune systemThe cells, tissues and organs that assist the body to resist infection and disease by producing antibodies and/or altered cells that inhibit the multiplication of the infectious agent and provide resistance to disease. becomes protected against an infection. The purpose of immunisation is to prevent people from acquiring infectious diseases and to protect them against the associated short and longer-term complications of the disease.
Vaccine refers to the material used for immunisation, while vaccination refers to the act of giving a vaccine to a person. Vaccines work by stimulating the body’s defence mechanisms against an infection. These defence mechanisms are collectively referred to as the immune system. Vaccines mimic and sometimes improve on the body’s protective response, helping the immune system detect and destroy the infection when it is encountered in the future without development of significant symptoms or complications.

The immune system
To understand immunisation, we need first to understand the way in which the human body naturally protects itself against disease.
Diseases come in many forms: some of the most lethal are caused by infectious pathogens such as bacteria GLOSSARY bacteriaA single-celled, microscopic organism without a distinct nucleus. , viruses GLOSSARY virusesViruses are submicroscopic infectious agents consisting of a nucleic acid (DNA or RNA) molecule surrounded by a protein coat. Viruses cannot replicate outside a living cell. and parasites. Once they have invaded the body, they begin to attack and multiply. To combat infection by these pathogens, the body's immune system can marshal two main lines of defence—innate or natural immunity GLOSSARY natural immunityImmunity that is present in an individual at birth prior to exposure to a pathogen or antigen which provide an initial response against infection. , and acquired immunity GLOSSARY acquired immunityAcquired immunity results from the development of antibodies in response to an antigen, as from exposure to an infectious disease or through vaccination. .
These two lines of defence have different characteristics:
- natural immunity has a more rapid response than acquired immunity;
- natural immunity responds in the same way to all infections by pathogens; acquired immunity responds in a specific way to each different infection;
- acquired immunity has a ‘memory’ of previous infections. There is some evidence that innate immunity can also have memory;
- natural immunity has the same level of response to each new infection; acquired immunity shows a much greater response to subsequent infections by identical microorganisms.
Vaccination is a form of innate and acquired immunity.
Often made up of killed or modified microbes, certain parts of microbes or even microbial DNA, vaccines trick the immune system into believing that an infection has occurred. The immune system then jumps in to action, attacking the (actually harmless) vaccine and thus preparing itself for any future invasions of the type of microbe contained within the vaccine.
Immunisation is designed to block specific infection. This means that we need to have a separate vaccine for each infection. At present there are six major vaccine-preventable diseases—pertussis, childhood tuberculosis, tetanus, polio, measles and diphtheria. The capacity of the immune system to respond independently to each infection also explains why the system cannot be overloaded or damaged by giving the full range of currently available vaccines, or by having multiple antigens in one vaccine preparation.
Benefits and risks
Who benefits from immunisation?
Individuals, communities and whole populations can benefit from immunisation.
An effective vaccine protects an individual against a specific infectious pathogen and its associated various complications. In the short term, the efficacy of a vaccine is measured by its capacity to reduce the overall frequency of new infections, and to reduce major complications, such as serious tissue damage and death.
All vaccines currently in use in Australia confer high levels of protection that are sufficient to prevent disease in the great majority of vaccinated individuals, and in the wider community. For example, the pertussis vaccine prevents disease in 85 per cent of recipients, while the measles vaccine prevents disease in 95 per cent of recipients. The remaining individuals may not be fully protected and remain at least partially susceptible to infection. This may be due to genetic factors, or to the presence of other medical conditions that impair the capacity of the vaccine recipient to mount a protective immune response.
Thus, in a given population, no vaccine will be 100 per cent effective: if a disease is prevalent in a community, some people who have been vaccinated may still contract it.
Recent studies have indicated that the new acellular whooping cough vaccine, while giving fewer side-effects, may be slightly less effective than the traditional vaccine made from a killed, whole microorganism.
An important feature of immunisation is that it brings benefits not only for the individual who receives the vaccine, but also for the entire population through a phenomenon called herd immunity.
Herd immunity GLOSSARY Herd immunityA form of immunity that occurs when the vaccination of a significant portion of a population (or herd) provides a measure of protection for individuals who have not developed immunity. occurs when a significant proportion of individuals within a population are protected against a disease through immunisation. This situation offers indirect protection to people who are not vaccinated, or who were but whose immune systems did not respond to the vaccine, by making it less likely they will come into contact with someone who is carrying the pathogen.
In the case of a highly infectious disease such as measles, more than 95 per cent of the population must be vaccinated to achieve sufficient herd immunity to prevent transmission if the disease recurs.
An additional benefit of vaccination is economic. Cost-effectiveness of community immunisation programs is determined by measuring the benefits—in terms of cost and quality of life—that result from preventing illness, disability and death, and comparing them with the costs of vaccine production and delivery to the population. A striking example is the benefits of the polio vaccination. In the first six years after the introduction of the vaccine, it was calculated that more than 150,000 cases of paralytic polio and more than 12,500 deaths were prevented worldwide. This represented a saving of more than US$30 billion annually in 1999 dollars.
Vaccination around the world
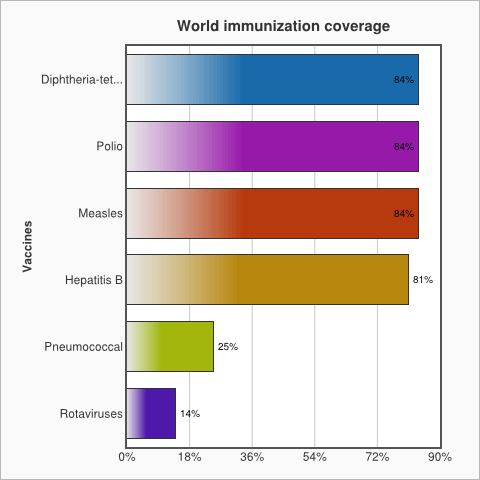
Despite these impressive figures, there is still work to do. Of the 21.8 million children around the world who are not fully immunised, 75 per cent of them live in just 15 countries.
In Australia, immunisation rates are high. Data from December 2014 shows that more than 92 per cent of five-year-olds are fully immunised.
What are the risks?
Vaccination is not completely risk-free. Like other medications, there can occasionally be side-effects, but the vaccines currently used in Australia provide benefits that greatly outweigh the risks. Before vaccines are made available, clinical trials with increasing numbers of participants are required to study safety. After vaccines have been introduced in to the community, safety monitoring continues.
The vast majority of side-effects that follow vaccination are minor and short-lived. The most common side effects for all vaccine types are ‘local’ reactions at the injection site, such as redness or swelling. More general ‘systemic’ reactions can include mild fever or tiredness. These reactions are outward signs that the vaccine is interacting with the immune system to generate a protective response. The nature of these reactions varies, depending on the type of vaccine given.
Serious side effects from vaccines are extremely rare. Potentially serious side effects, such as transient febrile seizures, have been reported after vaccination. However, such severe side effects occur much less often with the vaccine than they would if a person caught the infection itself. For example, about 3 in every 10,000 children who receive the MMR (Measles, Mumps, Rubella) vaccine develop a fever high enough to cause short-term seizures. In contrast, the risk of such a fever is more than 30 times greater among children who develop the disease—affecting about 100 in 10,000 children.
The frequency of side effects associated with some earlier vaccine preparations (no longer in use in developed countries such as Australia) was higher than with the current generation of vaccines. It is important to note that some alleged links between administration of certain vaccines and onset of diseases such as autism and autoimmune diseases have proven to be false.
Vaccine safety has been examined in great detail in recent years by expert committees such as those convened by the US Institute of Medicine. Their findings show that the risks of side-effects are generally extraordinarily low.
What vaccines are made of
Vaccines generally contain two major types of ingredients: antigens and adjuvants. Antigens are designed to activate adaptive immune responses which include antibodies and/or T-cells against a specific pathogen or its toxin. Adjuvants amplify immune responses more generally, especially innate immunity which is important for the induction of adaptive immunity.
Some vaccines comprise the killed whole pathogen (virus or bacteria) that the vaccine is designed to protect against. The virus is grown in the laboratory and killed by heat and/or chemicals to render it non-infectious. The injectable poliomyelitis vaccine is an example of this type of vaccine.
Other vaccines contain only components of the pathogen as their antigens. These components can be prepared by purifying them from the whole bacterium or virus, or by genetically engineering them. Engineered vaccines include the hepatitis B virus vaccine and the human papillomavirus vaccine.
Another group of vaccines is based on the toxin produced by the pathogen that causes the disease symptoms. The toxin is chemically treated to make it in to a harmless toxoid. The antibodies produced against this toxoid are still able to neutralise the toxin, and to prevent the disease from developing. Examples of this type include the tetanus and diphtheria vaccines.
Some vaccines do contain an infectious micro-organism. These are called live vaccines. These micro-organisms are an attenuated (less pathogenic) form of the pathogen that the vaccine aims to protect against. Examples include the injectable MMR vaccine, the oral polio vaccine and the chickenpox vaccine. Alternatively, a live vaccine may contain a naturally occurring organism that is closely related to the pathogen, but does not cause disease in healthy humans. An example is the BCG vaccine against tuberculosis and leprosy.
Eradicating disease
It is incredibly difficult to eradicate a disease… but not impossible. Global vaccination programs resulted in the successful eradication of small pox in 1980.
In 1988, the World Health Organization, in partnership with UNICEF and the Rotary Foundation began a public health campaign to eliminate all cases of poliomyelitis (polio). Following intensive immunisation programs, cases dropped from hundreds of thousands to only 291 in 2012—a massive reduction of over 99 per cent. However, eliminating that final 1 per cent has been incredibly difficult. Post 2012 polio has begun to re-emerge in some areas. Conditions in countries such as Syria, Pakistan and Cameroon have allowed the disease to gain a foothold once more, and it has spread quickly to Afghanistan, Iraq and Equatorial Guinea. This re-emergence highlights the importance of consistent vaccination programs and continuous monitoring to keep the disease in-check.
Future challenges
Vaccine researchers are now working to develop vaccines against acquired immune deficiency syndrome (AIDS), malaria and tuberculosis, which collectively cause more than five million deaths worldwide per year. These infections have so far eluded conventional vaccine development as they require both require a T cell as well as antibody response, but recent trials into human immunodeficiency virus (HIV) and malaria are proving promising. New technologies and innovative methods for clinical trials are constantly emerging too. This collective research is helping vaccine researchers to better address the needs in a 21st century world that is characterised by increased human life expectancy, emerging infections and poverty in low-income countries.
Conclusion
While there are some rare complications that can result from vaccination, a far greater risk will arise if the immunisation rate against these diseases begin to fall. It is only when immunisation rates are high that Australian children—and the wider community—will be protected against polio, diphtheria, whooping cough or tetanus, diseases that only a few decades ago were greatly feared. We have already had a taste of low immunisation levels with the 2010/2011 outbreak of whooping cough. We need a shot in the arm—or maybe several—if we’re to halt such diseases in their tracks.