Plasma: the liquid gold running through our veins
Expert reviewers
Essentials
- Plasma is the liquid component of blood.
- Plasma transports cells, proteins, hormones and vitamins around the body and removes waste products.
- Plasma also contains proteins which defend our bodies against invaders and help blood to clot.
- Donated, frozen plasma is used in clinical settings such as hospitals.
- Most donated plasma is used to make a range of essential pharmaceutical products, such as those used to treat people with immune deficiencies or bleeding disorders.
- Not enough plasma is donated in Australia to create all the medical products needed by Australians.
Do you give blood? Know your blood type?
Start talking blood and—as I discovered when I started asking around the Nova team—pretty soon everyone’s in on the conversation.
‘I’m Rh negative’, says Amy, at the next desk over. ‘If I get pregnant, they say I’ll need an injection so my body won’t reject the baby.’ Sharon, just back from maternity leave, usually donates blood regularly. ‘But I’m on a break for now,’ she says. ‘You can’t donate when you’re breastfeeding.’ Then there’s Hayley, who sits across the corridor. With an immune deficiency which makes her susceptible to infections and viruses, she relies on donated blood to keep her healthy, visiting the hospital once a month for a transfusion. Without it, she probably wouldn’t be able to come to work at all. But it’s not the red stuff Hayley needs. It’s a product made from the other part of blood—the sometimes forgotten, but vitally important, liquid component: plasma.
Blood’s not all red
Quick quiz: what colour is your blood? Unless you happen to be an octopus or a peanut worm, the answer is pretty sure to be red, right?
Well, not exactly. If we’re talking proportions, the majority of your blood—55 per cent, to be exact—is actually, well … kind of yellow. That’s because, while red blood cells give blood its rosy colour, they’re only one part of the picture. In fact, blood is made up of four components: red blood cells, white blood cells, platelets and plasma.
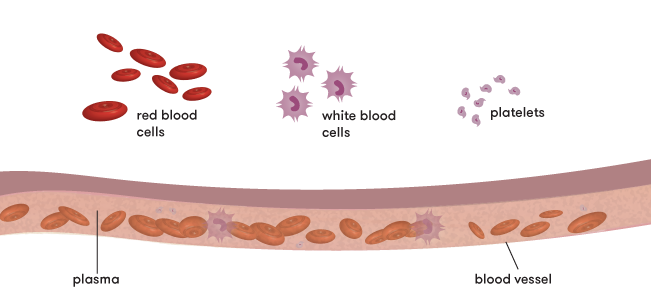
The main job of red blood cells is to carry oxygen around the body. It’s these cells that make our blood red. They get their colour from an iron-containing protein called haemoglobin which, when combined with oxygen, is bright red. (Just in case you’re wondering, octopus blood contains haemocyanin rather than haemoglobin. It’s an oxygen-transporting protein which contains copper and, when combined with oxygen, gives the blood a blue colour. The blood of peanut worms contains haemerythrin which turns violet-pink when oxygenated). White blood cells are mainly responsible for defending the body against infection. And platelets are small cell fragments which help your blood to clot by clumping together at the place of bleeding.
Important as they are, red cells, white cells and platelets aren’t going to do you much good if they can’t get from A to B. A red cell in a vein on its own is a bit like a kid on a waterslide without water. That’s where the yellow stuff—plasma—comes in. It’s the liquid portion which transports these cells, as well as proteins, hormones and vitamins, around your body.

What’s plasma for?
Lots of things. Plasma is mainly made up of water (around 92 per cent), helping to maintain our circulation: it fills up our blood vessels by flowing continuously—without it, a blood vessel would just collapse like a sad, floppy hose. Plasma also helps remove waste products from the body, by transporting them to the liver or kidneys, for example. And it carries heat from core tissues to other areas of the body like our hands and feet, helping us maintain our body temperature.
But plasma isn’t just the transporting liquid in our blood-vessel waterslide. Aside from keeping things flowing, it contains components that play important roles in the body—such as dissolved salts called electrolytes (yep, the same stuff you top up with sports drinks and those handy post-vomit ice blocks) which help regulate the blood’s chemistry and enable muscles to work properly.
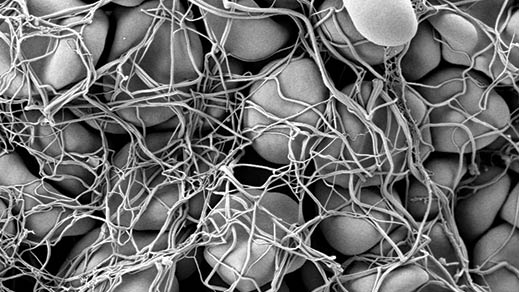
As well, plasma contains thousands of proteins which are vital to our body’s ability to function. Albumin is the most abundant of these. It’s made in the liver and keeps the right amount of fluid in your bloodstream (and out of your body’s tissues), as well as carrying important chemicals in your blood. Then there are globulins, of which there are three main kinds: alpha, beta and gamma. Alpha and beta globulins are made in the liver. Their functions include transporting various compounds around the body. Gamma globulins are made in the cells of the immune system and act as the body’s defence system. During an immune response, they help defend it against invaders such as viruses and bacteria. These defender proteins are also known as immunoglobulins, or antibodies. Fibrinogen proteins, also made in the liver, control bleeding by forming blood clots.
Here, have some of mine
As you’ll know if you’ve ever looked into donating blood, it’s not just the red stuff that can be donated—platelets and plasma from donors are also used for a range of medical treatments. The product which Hayley receives via her monthly transfusion, for example, is made from plasma. Indeed, plasma and plasma products are vitally important to many Australians’ quality of life. Yet at present, the amount of plasma donated in Australia falls short of what’s needed to create the intravenous immunoglobulin to treat people like Hayley. The shortfall has to be imported from overseas.
There are a couple of different ways you can donate plasma. The first is to donate whole blood (red cells, white cells, plasma and platelets), which is then separated out so that the different components, including the plasma, can be used to treat specific medical conditions. The second is to donate just plasma via a process known as plasmapheresis. This is where a machine takes your plasma and sends the rest of your blood back to your body. Not only does this enable more plasma to be collected (one donation by this method gets you about two to three times the amount of plasma as you’d get via a whole blood donation), but it also means that donors can donate more often without running low on iron.
The process goes something like this. A needle is put into your arm with a tube running from it into the plasmapheresis machine. A pump then draws the blood from your arm into a blood-separating kit in the machine. A small amount of anticoagulant is added to stop the blood from clumping together in the machine.
Inside the machine, your blood goes into a centrifuge where it gets spun around at high speeds. This separates the blood into layers: because plasma is lighter it ends up on the top layer, while the heavier red cells sink to the bottom. The machine is programmed to recognise the plasma, sending it into a special collection bag. Every so often the red cells are flushed back into your arm.
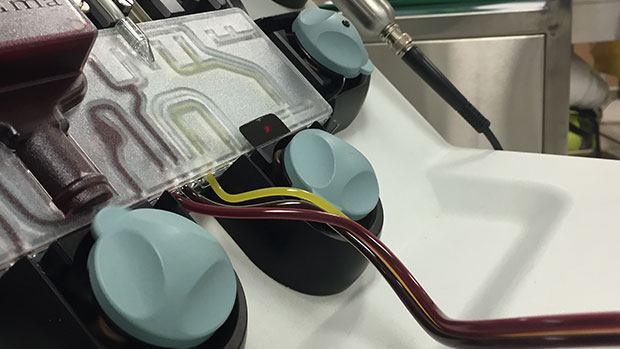
The whole cycle is repeated again, and again, until the desired amount of plasma (depending on your weight, height, and so on) has been obtained.
What happens to donated plasma?
It’s frozen for use in hospitals
Donated plasma can be frozen and kept for up to 12 months. This freshly frozen plasma is known, pretty sensibly, as fresh frozen plasma (FFP for short). Because it contains proteins which help with clotting, FFP can be used in clinical settings such as hospitals to treat major bleeding—for instance, in the case of a car accident or major operation.
There are two further products which can be made from FFP and used to prevent bleeding. Cryoprecipitate is one of these. It’s made from residues collected when frozen plasma is thawed at refrigerated temperatures and contains protein molecules which help blood to clot—the most important of which is fibrinogen. Cryoprecipitate is mainly used as a fibrinogen supplement for people who are low in fibrinogen and have a lot of bleeding, or who’ve undergone an invasive procedure. The other product made from FFP is cryo-depleted plasma: it’s basically what’s left once the cryoprecipitate has been taken out. It contains some other clotting factors that aren’t in cryoprecipitate. The main use of cryo-depleted plasma is for the treatment of a rare (but often fatal) blood disorder called Thrombotic Thrombocytopenic Purpura (TTP).

It’s used in pharmaceutical products
As important as FFP is for use in hospitals, most donated plasma is actually used for something else: the creation of plasma-based pharmaceutical products. If you have a bleeding disorder or an immune deficiency, you probably already know the importance of medical products made from plasma.
But what if you’ve ever needed a tetanus shot? Chances are, though you may not have realised it, you’ve also been the recipient a plasma-based product. The immunoglobulin products made from plasma provide “passive immunity”. They contain high levels of antibodies against certain infections which can help to protect an individual against the disease, but these antibodies only last for a number of weeks. They do not provide long-term immunity. Tetanus immunoglobulin, for example, contains high levels of antibodies against tetanus and can be used to protect a person who has sustained a tetanus-prone wound but has not previously been vaccinated. In these circumstances, the patient is usually given a tetanus immunoglobulin injection as well as the tetanus vaccine. This provides them immediate protection against tetanus as well as providing protection over the longer term.
So how exactly does donated plasma get turned into a whole variety of medical products? In Australia, after being donated and frozen, it’s sent to biopharmaceutical company CSL Behring. Here, it’s separated out by a process called fractionation. As we’ve seen, the different proteins in plasma have different functions—fractionation is where only the proteins that are needed to do a particular job are extracted so that they can be made into particular therapeutic products.
| Plasma-based product | Used for | Whole blood donations needed | Plasma donations needed |
|---|---|---|---|
|
Rh(D) Immunoglobulin-VF (also known as anti-D) |
Preventing haemolytic disease of the newborn (for Rh-negative pregnant mothers) |
0.1 |
0.04 |
|
Intramuscular Immunoglobulin |
Immunisation against hepatitis A, measles and poliomyelitis |
0.7 |
0.3 |
|
Albumin |
Treating patients suffering from shock due to blood loss |
2.7 |
1.2 |
|
Intravenous Immunoglobulin IVIg |
Treating some primary immune deficiency disorders |
7.8 |
3.5 |
| Antithrombin concentrate | Preventing blood clots during surgery or childbirth | 20.1 |
9.0 |
|
Factor IX concentrate |
Treating patients with inherited bleeding condition haemophilia B |
31.1 |
13.9 |
The first step in the fractionation process is testing the plasma for blood-borne viruses. Next, all the frozen plasma donations are put together and thawed out into a big plasma soup. The plasma is then passed through specialised stainless steel cylinders and separated into the various plasma products. Any viruses in the plasma are then inactivated, with each type of plasma product having its own specific viral inactivation steps. These might be pasteurisation, nanofiltration, solvent/detergent treatment, low pH incubation, etc. Some of the other manufacturing steps also contribute to the viral safety of the products.
Altogether, there are 15 medical products made in Australia using donated plasma. They fall into three main types: immunoglobulins, clotting factors, and albumin. Immunoglobulins are used to treat immune disorders such as primary or acquired immune deficiency. They’re also used to help the immune system fight off disease—for example, to prevent chickenpox in people with weakened immune systems. Clotting factors can be used to treat bleeding disorders in which blood doesn’t clot normally, such as haemophilia (though most patients with haemophilia A and B are now treated with recombinant clotting factors), and von Willebrand disease. Albumin is used to treat fluid loss or to supplement low albumin levels—for instance, where someone is suffering from shock due to blood loss.
And that injection my Rh negative colleague Amy will need if she has a baby? It’s made from plasma too.
Compatibility issues
When it comes to the red stuff, most of us know that getting the wrong type of blood, say, in a transfusion, is not a good thing. Donated blood needs to be compatible with the blood type of the person getting it—if not, the recipient’s body will identify it as an intruder and its antibodies will go on the attack.
But it may be news to you that plasma, too, needs to be compatible with the blood type of the person receiving it. That’s because each of the four main blood types (A, B, AB and O) have specific antibodies in the plasma. These antibodies are the body’s defence system, and will attack certain types of introduced blood.
Not getting it? Let’s take a step back.
If you have a particular blood type, this means that your red blood cells have certain kinds of antigens on them (antigens are sugars and proteins on the surface of our cells). My blood type is B positive, so my red blood cells have B antigens on them. Our bodies aren’t keen on letting in intruders they don’t recognise—after all, they could be dangerous viruses or bacteria—and will produce antibodies to fight them off. So, in my case, my body will attack blood that has an antigen that my blood does not have —that is, A-type blood. To carry out this defence job, my plasma contains anti-A antibodies.
Say my blood-donating colleague Sharon has A-type blood, and she wants to donate some plasma to me, a B-typer. Having A-type blood means she has anti-B antibodies on her plasma. If she donated plasma to me, the anti-B antibodies in her plasma would attack my red cells. Thanks, but no thanks.
AB blood type is the universal plasma donor—that is, people with AB blood can donate their plasma to anyone, no matter what the recipient’s blood type. That’s because AB blood, having both A and B antigens on its red blood cells, welcomes all visitors. It recognises all blood types, whether A, B, AB (AB has both A and B antigens) or O (O has no A or B antigens).
Liquid gold
Liquid gold—that’s the nickname given to plasma by some in the blood donation game. Not only does it keep things flowing and prevent our blood vessels from collapsing, it contains a plethora of hardworking proteins which stop us from bleeding uncontrollably and help fight off bacteria, viruses and other nasties. And it’s essential for the creation of pharmaceutical products for people like Hayley, whose own plasma cells can’t make these vital defence mechanisms. Yet, in Australia, not enough plasma is donated to create all the medical products needed.
Given all that, I ask her, why aren’t more Australians donating plasma? Is it a fear of needles? Or a simple lack of time? She thinks for a moment. ‘Maybe they just don’t know they can.’
So—now you know. No excuses.