3. Who benefits from vaccines?

Individuals benefit, in the short and long term
Efficacy
Efficacy refers to how well a vaccine performs in preventing new infections as it goes through scientific testing.
An effective vaccine protects an individual against a specific infectious disease and its complications. In the short term, vaccine efficacy is measured by its ability to reduce new infections. The longer-term goal is to reduce serious complications and death.2
All vaccines currently used in Australia produce high levels of protection that are enough to prevent disease in most vaccinated individuals. In countries where the use of vaccination is widespread, there has been a dramatic reduction in the number of people who become ill and die from formerly common and severe infections.3 For example, the whooping cough vaccine prevents disease in 85% of recipients, while the measles vaccine prevents disease in 95% of recipients from the first dose alone.48 The remaining proportion of individuals may not be fully protected and remain at least partially susceptible to infection. This may be due to genetic factors, or to the presence of other medical conditions that affect their ability to mount a protective immune response to the vaccine. These people are also protected when herd immunity has been achieved (see ‘The community at large benefits’ below).
Booster doses of some vaccines are required to maintain protection
Examples of vaccines that require booster doses include whooping cough, tetanus, and polio vaccines, as well as conjugate pneumococcal and meningococcal vaccines. In contrast, a single course of others, such as the hepatitis B vaccine, appears to be sufficient to provide lifelong protection.
After the first immunisation, a small and brief response occurs. When additional (booster) doses are given, memory lymphocytes created during the initial response are switched on to generate a much more rapid and longer lasting protective response. The graphic below shows the levels of antibodies from B cells after first and booster vaccinations.17
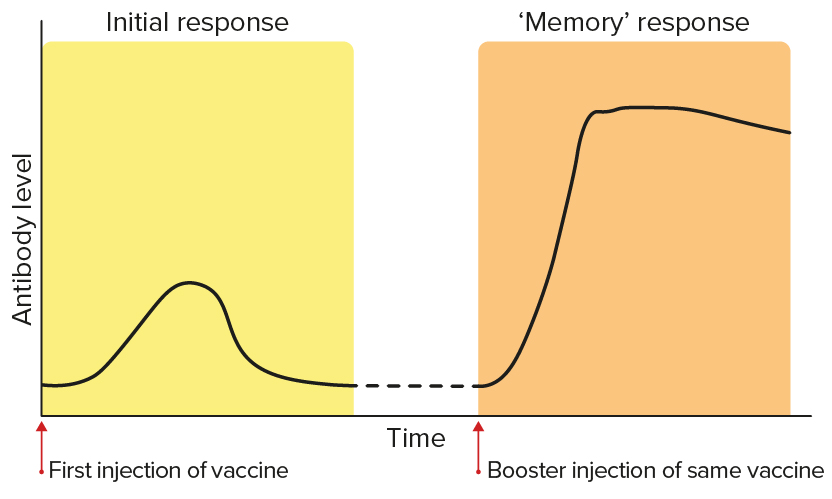
The levels of antibodies from B cells after first and booster vaccinations.
Vaccines can protect against long-term complications of infections
Encephalitis
Encephalitis is inflammation of the brain.
By preventing infection, vaccines can also prevent long-term complications associated with chronic infections, where the pathogen persists in the body after the initial infection has passed.
Certain viruses can cause dormant infections that persist in the body for years and cause long-term problems. Such persistent infections can eventually lead to chronic damage to infected organs (such as encephalitis induced by measles, or cirrhosis of the liver caused by hepatitis B or hepatitis C virus infection).49–51
Persistent viral infections can also lead to late complications such as cancer. For example, hepatitis B can lead to liver cancer and liver damage, and human papilloma virus can cause cancers including cervical and anal cancers.52–54 Vaccines are available to protect against these diseases.
Even if an individual has already been exposed to a disease, vaccines against that disease can still be beneficial in some cases, such as the chickenpox vaccine. This vaccine protects against the development of a long-term complication of the infection, shingles. Shingles is a debilitating condition characterised by the appearance of painful blisters on parts of the skin above nerves where the chickenpox virus has lain dormant since infection in childhood. Adults who had chickenpox in childhood can be given a high-dose chickenpox vaccine to boost immunity, resulting in a substantial reduction in their risk of developing shingles in the future. This is typically offered to elderly people, who are at higher risk of complications from shingles.55
The community at large benefits
Herd immunity occurs when a significant proportion of individuals within a population are protected against a disease through immunisation. This offers indirect protection for people who are still susceptible to the disease, by making it less likely that they will come into contact with someone who is carrying the pathogen.
Most vaccines not only benefit the individual who receives the vaccine but the entire population through a phenomenon called herd immunity.2
Herd immunity occurs when a significant proportion of individuals within a population are protected against a disease through immunisation. This situation offers indirect protection for people who are still susceptible to the disease, by making it less likely that they will come into contact with someone who is carrying the pathogen. Vaccination is the best way to create the right conditions for herd immunity to develop.
As well as protecting unvaccinated individuals, herd immunity benefits the small proportion of people who fail to respond adequately to vaccination or are unable to be vaccinated for medical reasons.56
In the case of a highly infectious disease such as measles, more than 95% of the population must be vaccinated to achieve sufficient herd immunity to prevent transmission if the disease recurs.
Vaccines across the life span

Newborn babies
The body’s immune system begins developing before birth. In the period during and soon after birth, when the functions of the immune system are still maturing, newborns are protected against many, but not all, serious infections by antibodies from their mother. This protection usually lasts for about four months.
Babies and children
As the early protection provided by the mother’s antibodies fades away, a child’s innate and adaptive immune systems start to mature and develop a memory of infections.57 They are more vulnerable to some infections at this age as their immune system is still maturing. However, their protection against pathogens grows throughout this time.
Children also have protection from early vaccinations. The current immunisation programs are designed to balance the ability of the child’s immune system to respond to the vaccine against the risk of the child getting the infection.
Adults
Adults require booster doses of some vaccines, such as tetanus, to maintain adequate levels of immunity throughout their life. Additional vaccines may be required in adulthood if the person plans on travelling overseas.
Not every person has a normally-functioning immune system, and some have primary or secondary immune deficiencies. A primary immune deficiency is one a person is born with, and a secondary immune deficiency is one that a person acquires from a disease or treatment, such as chemotherapy. Some people may be immunosuppressed from a disease or treatment, such as people receiving treatment for autoimmune diseases or cancer. These people may not be able to produce a strong immune response following vaccination and may rely on herd immunity to be protected from acquiring diseases.
Pregnancy
Maternal antibodies
Maternal antibodies are antibodies produced by a mother and transferred to the fetus.
Maternal antibodies cross the placenta into the baby’s circulation before birth and are also present in the mother’s breast milk. If the mother has been vaccinated or has recovered from infection during pregnancy, the amount of antibodies transmitted to the baby can be sufficient to ensure complete protection. On the other hand, if the mother’s infection (particularly with the pathogen that causes whooping cough) or immunisation occurred a long time ago, the antibody levels and protection may be lower.
Some vaccines, including inactivated vaccines, are considered safe to be given during pregnancy. The rates of side effects among pregnant women are similar to those in the general population. No link has been established between vaccination with inactivated vaccines in pregnancy and birth defects. The use of inactivated vaccines in pregnancy is particularly desirable for infections such as influenza and whooping cough that affect pregnant women or their babies more severely than the general population. This is because vaccination during pregnancy protects the mother against infection and provides protection to the baby as a result of the transfer of maternal antibodies.
Live attenuated vaccines, such as the MMR vaccine, are not recommended during pregnancy, as the live viruses could theoretically be transmitted from pregnant mothers to their baby. However, there is no evidence of increased birth defects in children whose mothers inadvertently received live attenuated vaccines while pregnant.
Older adults
Older adults, particularly people over 65, will experience a progressive decline in immunity as they get older. This means that they are more susceptible to infection and less responsive to vaccines.
Infection due to influenza, varicella-zoster viruses (causing chickenpox and shingles), SARS-CoV-2 (causing COVID-19) and Streptococcus pneumoniae can cause severe illness in older adults. Most of these diseases also lead to increased risk of death in older adults.
Special vaccines designed to work better with the immune system of older adults are made in two main ways:
- Developing new types of adjuvants to stimulate the immune response more effectively
- Increasing the amount of antigen included in the vaccine
Vaccines can control, eliminate and eradicate diseases
When a large proportion of a community is immunised, it can lead to a situation where there are very low disease levels in that population. This is referred to as control of the disease.
Even more effective and prolonged vaccination programs can result in interruption of transmission in the population for long enough to eliminate the disease. However, even when high levels of community coverage with a vaccine are achieved, infection may be reintroduced, such as by unvaccinated travellers. In Australia, isolated outbreaks of infectious diseases such as measles have been attributed to transmission from unvaccinated travellers.
Once a high degree of control is achieved worldwide, it is theoretically possible to eradicate an organism and the associated risk of infection, provided there is no other animal that can carry the infection and transmit it back to humans. This was achieved with smallpox in the 1970s. There is hope that such a goal may also be achievable for polio and measles, since (as with smallpox) humans are the only hosts. Of the three strains of polio, two strains have already been eradicated. Compared with 350,000 cases in 1988, only 33 polio cases were reported worldwide in 2018.
Vaccination brings economic benefits
In the first six years after the introduction of the polio vaccine worldwide:
- more than 150,000 cases of paralytic polio were prevented
- more than 12,500 deaths from polio were prevented
- more than US$30 billion per year (in 1999 dollars) was saved.58
The cost-effectiveness of community immunisation programs is measured by determining the benefits that result from preventing illness, disability and death, and comparing them with the costs of vaccine production and delivery to the population.
Better health, hygiene and vaccination reduces infections
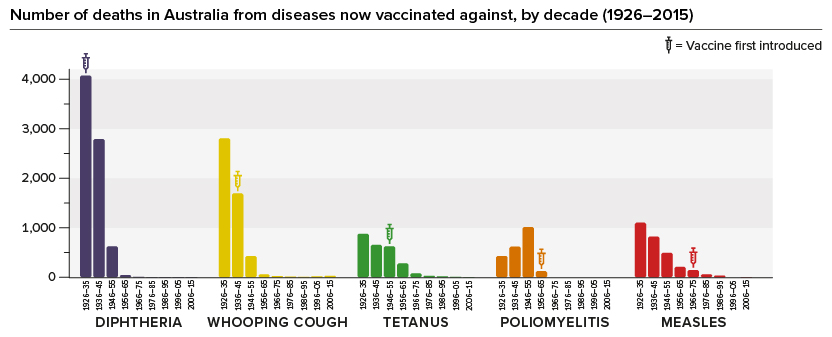
Hygiene and healthcare improvements, such as widespread availability of antibiotics and better overall medical support systems, have reduced deaths from all diseases. However, vaccines have had an additional substantial impact: deaths in Australia from diphtheria, whooping cough, tetanus, polio and measles have all dramatically declined or disappeared since vaccines were introduced.
The introduction of the Haemophilus influenzae type b (Hib) vaccine in 2003 and the meningococcal type C vaccine in 2004 led to a very rapid and noticeable decline in the number of severe and sometimes fatal infections. This effect cannot be attributed to any change in living conditions or medical treatment.





